Incontinence-associated dermatitis (IAD) is frequently found in patients with diarrhoea or stool incontinence. This is as a result of contact dermatitis to the skin in the perianal and perineal area. There are a number of terms that can be used to describe IAD. These include: perineal dermatitis, perineal rash, nappy rash, nappy dermatitis, irritant dermatitis, moisture ulcers and moisture lesion.1
IAD is seen much more frequently in older people, but can be found throughout all age groups. It causes pain, burning, tingling and pruritis and, as a result, patients with IAD often develop insomnia, which leads to a decreased quality of life (QoL) and a disruption to their daily activities. This can in turn spiral into a vicious downward cycle if timely control cannot be achieved. As the frequency of stool incontinence increases, the more severe the IAD becomes and the greater the discomfort the patient experiences.
IAD can be graded into two categories.1 Grade 1 IAD presents with erythematous skin, but the skin is intact. Grade 2 IAD shows erythema of the skin but there is associated breakdown of the skin. This predisposes the patient to developing secondary bacterial or fungal infection and at the same time increases their risk of developing pressure injuries.
The primary goal of managing a patient with IAD is to manage the incontinence. However, at the same time, it is important to stop the progress of the dermatitis. Previous studies have shown that skin barrier products such as petrolatum,2,3,4 zinc oxide,2,4,5 dimethicone,2,4,6,7,8 acrylate polymer,2,4,6,9,10 and cyanoacrylate skin bonding polymer2,4,6,10,11,12,13,14 are effective. However, at present there is no consensus on what the optimal form of medication should be. Some of the skin barrier sprays and powders that are described are often costly. Our study looked at using a combination of topical antibiotic and topical antifungal medication. This mixture provided an adequate barrier dressing as well as containing antibacterial and antifungal elements. It is cheap and effective, and is well suited for use both in the hospital as well as in the home setting. The aim of this study was to assess the effectiveness of this form of management.
Methods
Patients with grade 2 IAD treated with a combination of topical antibiotic (Biomycin, CBC Biotechnological and Pharmaceutical, Taiwan) and topical antifungal (Clotrimazole, Sinphar Group, Taiwan), between January 2017 and January 2019, were included in this retrospective study. The diagnosis of grade 2 IAD was only made if there was consensus between the physician in charge of the patient and the wound care sister (World Council of Enterostomal Therapists, WCET certified).
All patients who had undergone any other methods of management of their IAD were excluded from the study. Patient demographic data collected included age, sex, diagnosis, body mass index (BMI), comorbidities, grade of IAD and the surface area of the skin involved.
Patients were reviewed fortnightly until the wounds had healed, the patient was discharged or until death. Statistical analysis, using Chi-square and paired t-test, was carried out to assess the rate of wound healing.
Ethical approval and patient consent
The Institution Review Board of our hospital approved this study. Patients gave oral consent to inclusion in the study and for the taking of photographs.
Results
A total of 253 patients were diagnosed with IAD in the study period, 76 of whom fulfilled the inclusion criteria and were enrolled in into this study. There were 39 men and 37 women with a mean age of 74 years (range: 36–96 years). In 58 (76%) patients, the area involved was >50cm2, in 13 (17%) patients the area involved was 20–50cm2 and in five (7%) patients the area involved as <20cm2.
The patients often had multiple comorbidities. There were six (8%) patients with cancer, eight (11%) patients with cardiovascular disease, eight (11%) patients with cerebrovascular disease, 19 (25%) patients had pneumonia, 15 (20%) patients had other associated infections in the body, 13 (17%) patients with gastrointestinal disease, three (4%) were orthopaedic patients, two (3%) patients had urinary tract infection and two (3%) patients had immunodeficiency. The mean BMI of patients was 22.5kg/m2 (range: 13.81– 32.3kg/m2). The mean number of days treated was 10.3 (range: 1–53). Table 1 shows the demographic data for patients in the study.
Table 1. Patient demographics and results (n=76)
| Comorbidity | Number (%) |
|---|---|
| Cancer | 6 (8) |
| Cardiovascular disease | 8 (10) |
| Cerebrovascular disease | 8 (10) |
| Gastrointestinal disease | 13 (17) |
| Pneumonia | 19 (25) |
| Urinary tract infection | 2 (3) |
| Immunodeficiency | 2 (3) |
| Unspecified infections | 15 (20) |
| Orthopaedic conditions | 3 (4) |
| Surface area involved, cm2 | |
| <20 | 5 (7) |
| 20–50 | 13 (17) |
| >50 | 58 (76) |
| Healing of surface area | |
| Complete healing of area involved | 46 (61) |
| >50% surface area improved | 17 (22) |
| 0–50% surface area improved | 7 (9) |
| No improvment | 5 (7) |
| Surface increased | 1 (1) |
A total of 46 (61%) patients showed total healing of their IAD at discharge, 17 (22%) patients showed an improvement of >50% of the involved area, seven (9%) patients showed an improvement of 0–50%, five patients (7%) showed no improvement, and one (1%) patient showed an increase in the area affected by IAD. In the one patient where the affected size actually increased, he had terminal pancreatic cancer with liver cirrhosis. He developed persistent melaena due to a low platelet count and ultimately died 28 days after admission. In the five patients where there was no change in the affected area, one patient changed from IAD grade 2 to grade 1, two patients died soon after admission, and two patients were discharged after three days and were lost to follow-up.
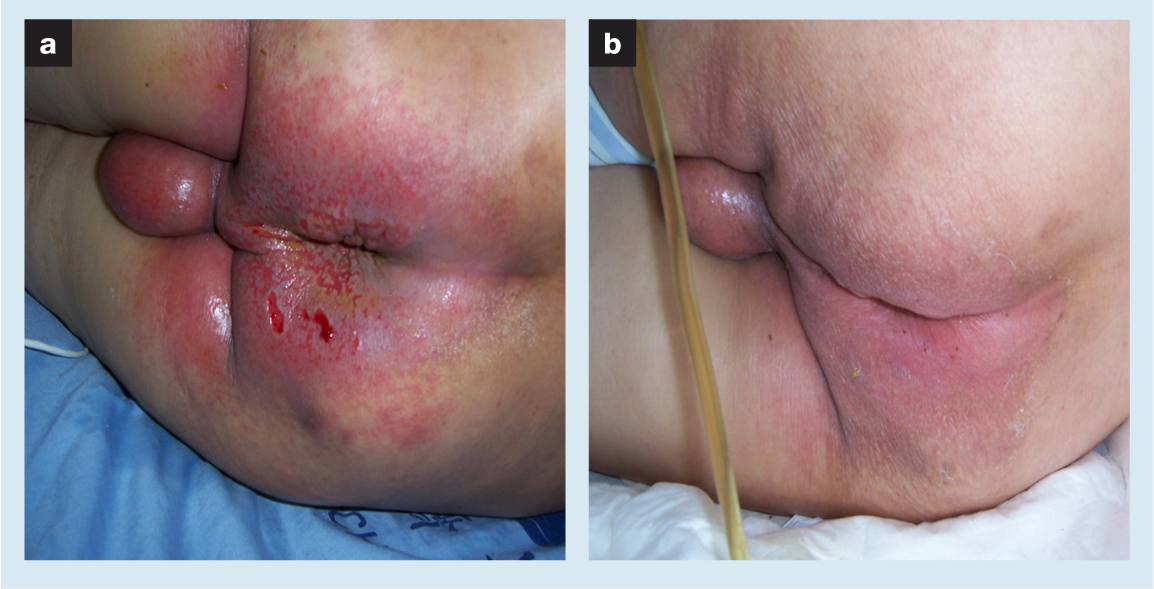
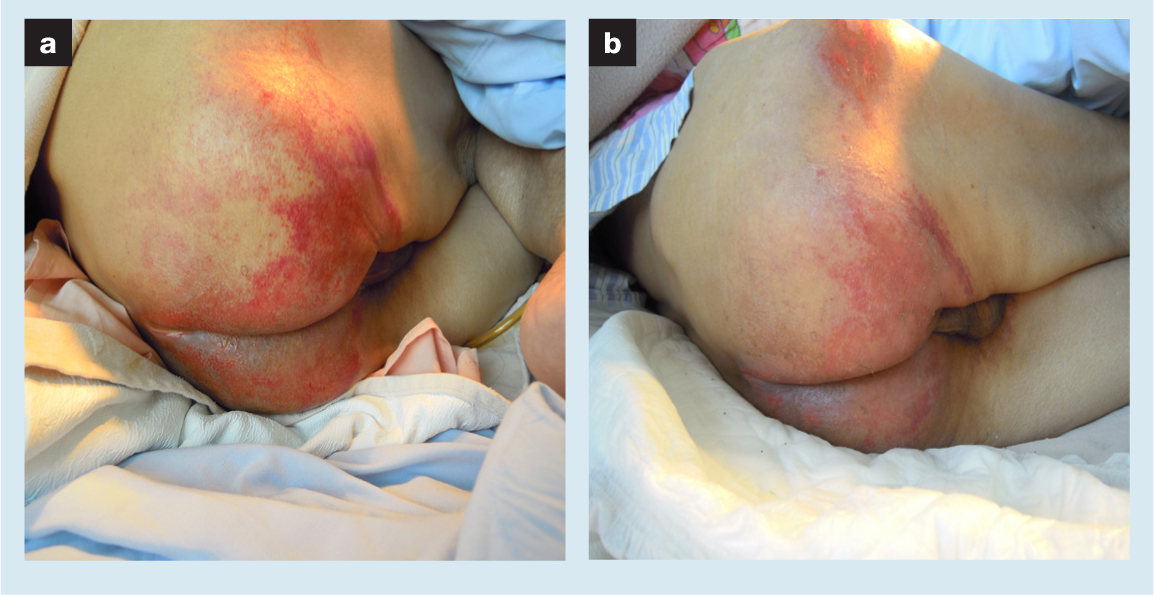
Fig 1 and Fig 2 each show cases of patients with incontinence-associated dermatitis.
Discussion
IAD results in skin erythema, breakdown and ulceration. It is associated with pain and often leads to extreme patient discomfort. These wounds often become infected due to being in contact with urine and faeces. Care for these patients can at times be challenging.
The basis of all forms of management for IAD is some form of barrier treatment in order to prevent the skin from coming into contact with irritant bodily fluids (urine and faeces). Clinically, there are many options.
Zinc oxide pastes offer good protection against irritants, but they are thick and difficult to apply.2,4,5 Once applied, they are exceedingly adherent to the skin and problematic to remove. It may interfere with primary dressing adherence and absorption. At the same time, it can inadvertently spread into the wound, interfering with other antimicrobial ingredients applied.
Another barrier product commonly used is a combination of zinc oxide with talcum powder.2,4,5 It has a thick consistency that helps keep the barrier surface intact during ongoing exposure to liquid stool. However, due to the talcum powder, it can make the paste feel gritty. Due to this gritty texture, it is at times extremely uncomfortable and painful on application, during the time it is applied, as well as during cleansing and removal. Liquid stool can become embedded into the surface of the product, necessitating frequent removal and cleansing. This can increase the likelihood of mechanical trauma to an already damaged, fragile skin. Pastes also transfer onto incontinence pads and bed linen, diminishing the barrier protection and compromising the effectiveness of the absorbent products. A further disadvantage is that it is often difficult to mix the zinc oxide and talcum powder to the right consistency and ratio.
A further barrier product frequently used is petrolatum (Vaseline, Unilever plc., UK).2,3,4 Its advantages are that it forms a seal over the skin to reduce transepidermal fluid loss. It shows optimal effect when applied to slightly dampened skin. It has thickening properties to protect against mechanical damage and serves as a physical barrier against irritants. This product offers good protection against irritants, avoids maceration and can often be mixed with zinc oxide for extra protection. However, it leaves a greasy residue that interferes with primary dressing adherence and absorption. It may build up in the pores, trap dirt and bacteria, therefore increasing the risk of folliculitis. A further disadvantage is that it may also liquefy under heat. A major complaint is that it is too greasy and often not well tolerated by older people and male patients.
Dimethicone is another product often used.2,4,6,7,8 It is permeable to water vapour and allows the evaporation of perspiration, minimising the risk of miliaria (heat rash). It conforms well to the periwound area or to the at-risk skin. It is easy to spread and feels less greasy on the skin. However, a downside is that it may inadvertently get into the wound, which is a concern given that the product is not indicated for use in open wounds.
Film-forming polymers form a mechanical barrier over the periwound surface.2,4,6,9,10 They are thin and not messy to apply. They also allow adherence of wound dressings and protect against skin tearing during dressing changes. These polymers have an alcohol-free formulation resulting in less pain during application and when applied. They resist being washed off, resulting in potentially fewer applications. However, in some patients, due to certain organic solvents contained in the polymers, they may cause stinging and irritation. The aerosol application can cause inhalation problems as well as being a fire hazard. Much of the applied liquid evaporates, leaving a very thin, insubstantial film when compared with cyanoacrylates.
Cyanoacrylate formulations create a moisture-resistant barrier on the skin.2,4,6,10,11,12,13,14 They protect against friction-induced skin damage when in skin barrier formulations. They do not require a solvent, so all of the applied liquid turns into a barrier. They bond to the skin via polymerisation in situ and so are resistant to being washed off or being prematurely removed. They need only be applied every third day, which saves nursing time, and are easy to apply if the patient is in the home setting. However, in some patients, if the cyanoacrylate is not allowed to dry properly before putting on a diaper, the diaper can adhere to it, causing pain when removed. The main drawback is that cyanoacrylates are somewhat expensive and, some individuals may experience an allergic response to the cyanoacrylates. This product is not suitable for application in the presence of deep, open, bleeding, infected wounds and in second- or third-degree burns.2,4,6,10,11,12,13,14
In our hospital, we used use a combination of topical antibiotic and zinc oxide before our current management using a combination of topical antibiotic and topical antifungal medicines. The benefits of using topical antibiotic and zinc oxide were that the antibiotics could prevent infection and the zinc oxide provided a good barrier function. However, the main disadvantage was that patients with persistent diarrhoea tended to develop fungal infection of the affected area.
The advantages of using the combination of topical antibiotics and topical antifungal were that it could prevent bacterial as well as fungal infection. Both medications were easy to apply and were not an irritant to the skin. Both medicines were in an ointment form that was easy to remove with minimal friction injury to already fragile skin. This combination did not contain topical steroids and so would not interfere with the rate of healing. However, the main reason for its use was that both medications were cheap, easily accessible and were paid for by the national insurance system of Taiwan. The patients did not have to incur extra medical expenditure when using them. The main disadvantage was that this combination did not offer any form of barrier function, and so it was necessary to reapply the topical medication every time the patient had a bowel movement.
There are already commercially available products that contain neomycin, nystatin, triamcinolone acetonide and gramicidin that are also cheap, readily available and are paid for by the national insurance system. However, these are formulated as a relatively thicker cream. This makes it difficult to apply evenly over the affected area. It can also cause a pale yellowish discolouration of the skin which can interfere with the interpretation of the rate of healing during regular assessment of the underlying skin condition.
Limitations
The limitations of this study were that it was retrospective in nature and we did not have a control group with which to compare the effectiveness of our method. We did not use a perineal assessment tool to measure the risk of perineal skin injury and did not use the Braden scale to predict the risk of developing a pressure injury.
Conclusion
In this study, the use of a combination of a topical antibiotic and topical antifungal medication was effective in the management of grade 2 IAD. It was cheap, easy to apply, easy to remove and easily accessible. This made the combination easy and effective to use by the patient's family as well as by the hospital nursing staff.
Reflective questions
- What are the symptoms and signs associated with incontinence-associated dermatitis (IAD) and what are the possible complications?
- What forms the basis for the management of IAD?
- What are the most effective barrier products available for IAD management?
