Surgical site infection (SSI), ranging from superficial, deep and to the organ space, is one of the major predictors for morbidity and mortality in patients undergoing thoracic surgery. Care to accelerate SSI healing is taken to shorten the patient's hospital stay and to reduce costs. The application of vacuum-assisted closure (VAC) into the pleural space in thoracic patients is not well established in the literature.1 It is believed that VAC is a revolution in the management of SSI. It is a special form of local therapy that uses negative pressure.
In this study, the use and safety of a VAC device and its deep application in patients with various thoracic pathologies were examined, and our experience of introducing part of the VAC system into the pleural space described.
Method
A retrospective chart review for all patients who were admitted under thoracic surgery in a university hospital in Saudi Arabia between July 2014 and July 2018, and who developed an SSI. Patients were excluded if they had a superficial SSI, were paediatric patients, patients in whom VAC was applied in the non-thoracic area (such as the abdomen) and patients who had prophylactic application of VAC (V.A.C GRANUFOAM SILVER dressings, 3M+KCI, US).
SSI diagnosis was confirmed by radiography and cultures from the wounds. Once the VAC device was applied, patients received an initial intermittent negative pressure of 80mmHg that was gradually increased to 120mmHg. This was accompanied by daily chest X-ray to assess lung expansion.
Ethical approval and patient consent
Ethical approval was secured from the local review board committee. As this was a retrospective study, patient consent was not required.
Results
Patient demographic data are summarised in Table 1. A total of 12 patients (seven male and five female) were included in our study. Mean age was 41.2±14.9 years. Surgical intervention and length of VAC application is described in Table 2.
Table 1. Demographics of patients who received vacuum-assisted therapy (n=12)
| Character | Patients, n (%) |
|---|---|
| Sex | |
| Female | 5 (42) |
| Male | 7 (58) |
| Age, years, mean±standard deviation | 41.2±14.9 |
| Comorbidities | |
| Pneumonia | 4 (33) |
| Diabetes | 3 (25) |
| TB pleural effusion | 2 (16) |
| TB lymphadenopathy | 2 (16) |
| Hypertension | 1 (8) |
| Dyslipidaemia | 1 (8) |
| Acute coronary syndrome | 1 (8) |
| Hypothyroidism | 1 (8) |
Table 2. Surgical intervention and length of vacuum-assisted closure (VAC) therapy
| Number | Age, years | Diagnosis | Procedure | Local postoperative complication | Surgical management | Length of VAC after surgery, days* | Length of hospital stay, days |
|---|---|---|---|---|---|---|---|
| 1 | 26 | Stage III empyema | Thoracotomy and decortication | Deep surgical site infection and dehiscence | Debridement | 21 | 24 |
| 2 | 49 | Stage II empyema | Thoracotomy and decortication | Deep surgical site infection and dehiscence | Debridement | 4 | 32 |
| 3 | 56 | Recurrent hiatal hernia | Thoracoabdominal hiatal hernia repair + biological mesh | Oesophageal leak | Debridement of the whole wound | 30 | 48 |
| 4 | 46 | Stage III empyema | VATS (conversion thoracotomy + decortication) | Deep surgical site infection due to infected haemothorax | Debridement of the wound | 13 | 20 |
| 5 | 44 | Recurrent chondrosarcoma of chest wall | Resection | Recurrent discharging sinus with deep collection | Debridement of the wound post-resection | 14 | 15 |
| 6 | 23 | Right chest wall granuloma | Excision | Deep surgical site infection and dehiscence | Debridement | 5 | 7 |
| 7 | 47 | Coronary artery disease | CABG | Infected massive haemothorax | Thoracotomy + haematoma evacuation | 40 | 162 |
| 8 | 18 | Pectus excavatum | Nuss procedure | Serosanguinous discharge with deep collection | Removal of retrosternal bar | 12 | 26 |
| 9 | 62 | Right sterno-clavicular osteomyelitis | Right sterno-clavicular resection | Recollection and infection | Debridement | 15 | 30 |
| 10 | 61 | Tracheoesophageal fistula | Tracheoesophageal fistula repair | Mediastinitis | Debridement | 14 | 192 |
| 11 | 30 | Pott's disease | Surgical drainage of back abscess and debridement | Non-healing back sinus with deep collection | Debridement | 10 | 31 |
| 12 | 33 | Right stage II empyema | VATS decortication | Surgical site infection and dehiscence | Debridement | 9 | 24 |
VATS—video-assisted thoracoscopic surgery; CABG—coronary artery bypass graft surgery
SSI was diagnosed according to the primary diagnosis including: empyema, tuberculosis, neoplasm, inflammation, trauma or the presence of a foreign body.
A patient presented with recurrent discharging sinus with deep collection after multiple recurrent chest wall chondrosarcoma resection and reconstruction using cement graft. At five days postoperative, the patient developed an SSI. Debridement of the wound post-resection, drainage of the collection and application of a VAC dressing were carried out. The wound infection was treated successfully using VAC dressing for 14 days.
A 19-year-old patient underwent modified Ravitch procedure for pectus excavatum which was complicated postoperatively by SSI. VAC dressing was applied over 10 days, and the patient made a smooth recovery.
In five (42%) of the 12 patients, SSI was related to post-decortication for advanced empyema. Most of these empyema cases (n=4, 80%) were treated via an open approach (i.e., thoracotomy and decortication); the other one (20%) with video-assisted thoracoscopic surgery (VATS). In one of the five patients, an infected haemothorax and empyema complicated a coronary artery bypass graft surgery procedure. In this patient, the thoracotomy wound SSI was effectively managed with VAC dressing over a period of 40 days.
A non-healing back sinus with deep collection developed as a complication in one patient with post-incision and drainage of Pott's disease with a back abscess. Debridement was carried out and the wound improved with obliteration of the sinus after 10 days of VAC dressing.
In two patients, SSI was related to oesophageal pathology, one of whom presented with mediastinitis and septicaemia due to tracheoesophageal fistula. Post-surgical repair of the fistula was well managed with VAC dressing for 14 days. However, the patient remained in the hospital for a total of 192 days.
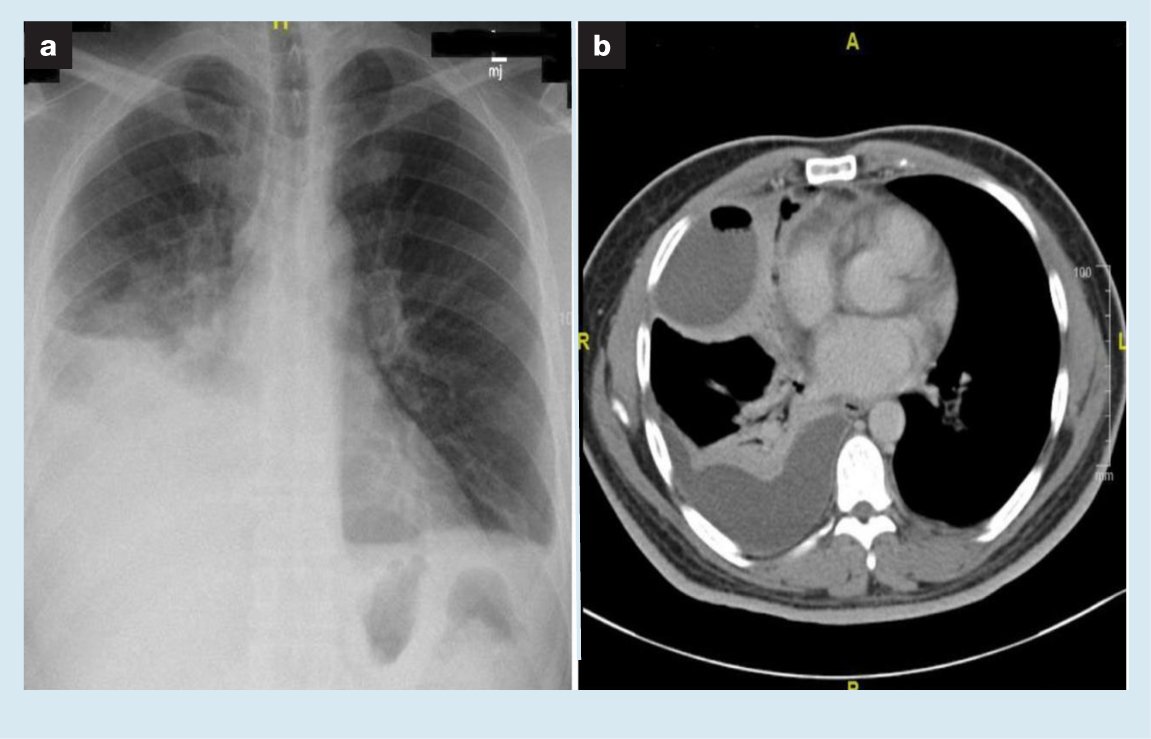
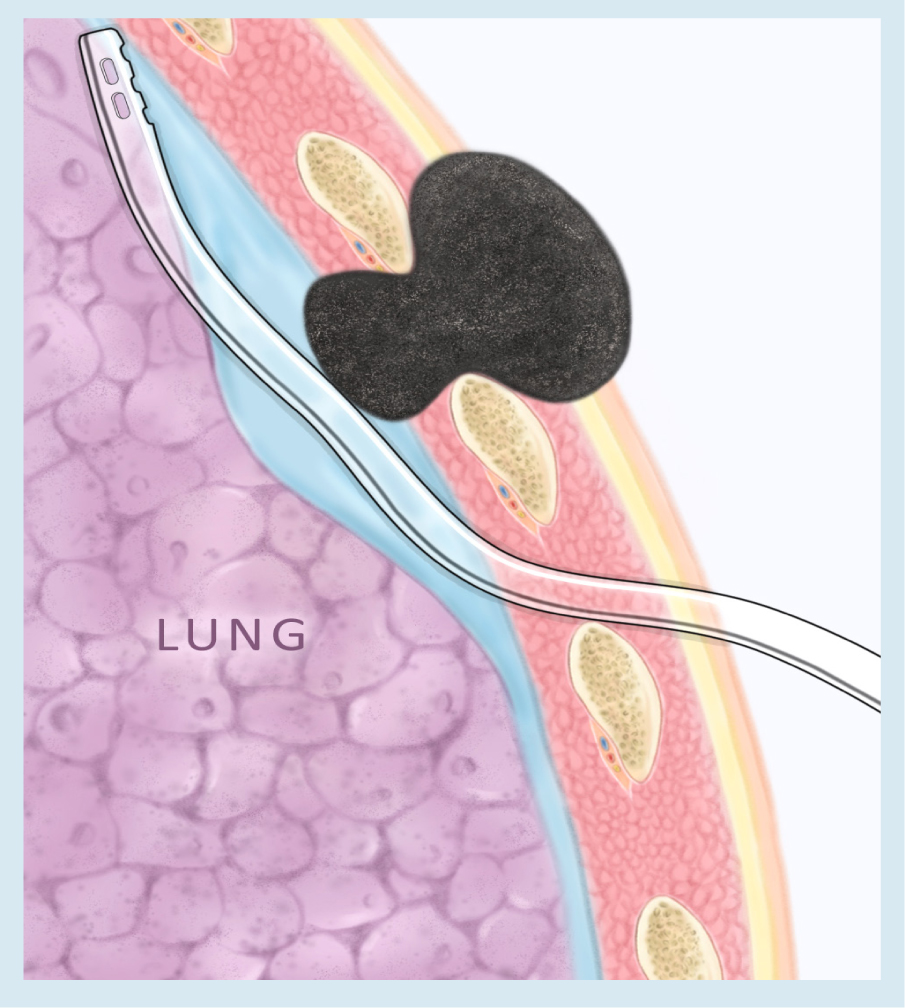
The majority of recruited patients received a deep application of VAC in which the sponge component was introduced into the chest wall wound extending to the level of the intercostal space, aided by immediate release oral and intravenous (IV) morphine (Fig 1). However, the technique was modified in two patients with empyema (Fig 2). In one patient, the sponge was inserted into a much deeper level so as to be partially intrapleural (Fig 3). This position allowed the sponge to act as a suction to the intrapleural infected content. In the second patient, a similar technique was used but over a chest tube inside the pleural space, piercing the chest wall from another intercostal level away from the wound (Fig 4). Both cases were performed under general anaesthesia. These techniques proved to be successful in both patients.


The average duration of VAC application was 14.3±9.7 days and the average vacuum pressure was between 100–125mmHg. Different microorganisms were isolated from the wounds. These were: Acinetobacter baumannii (n=3, 25 %), Staphylococcus epidermidis (n=2, 17 %), Pseudomonas aeruginosa (n=3, 25 %), Serratia marcescens (n=1, 8 %), Providencia stuartii (n=1, 8 %), Candida albicans (n=1, 8 %) and Proteus mirabilis (n=1, 8%). IV antibiotics were given according to culture and sensitivity. The VAC dressing was changed every 3–4 days. Both VAC and IV antibiotics were continued until resolution of local signs of infection and appearance of healthy granulation tissue filling the space. At this stage, the dressing was changed to topical wound care products. All patients showed good outcomes in terms of SSI resolution except in one case of mortality due to septicaemia and multiorgan failure.
Discussion
VAC is a therapeutic technique which can be used for a wide variety of infected and non-infected wounds, either acute or hard-to-heal.1,2,3 It is an evolving therapy method and its indication for use is constantly expanding. Both superficial and deep wounds can be treated with VAC.4 The device works by negative pressure which enhances local microcirculation, sucks away excess interstitial fluid and reduces the local bacterial load.5 Its first use in the management of postoperative wound infections in patients who had undergone decortication for post-lobectomy empyema was reported in 2006.6
VAC was considered an acceptable alternative in the management of postoperative space complication in thoracic surgery.7 Empyema necessitans is a challenging comorbidity.7 In such a case, VAC has been considered an effective treatment as an alternative for a debilitating thoracoplasty procedure.3 It has a role in minimising the surgical procedure required for empyema.8,9
The technique's safety and outcomes are not well studied in the literature. In the few studies that have reported on this, Rocco et al. concluded that the application of VAC was safe and associated with a decreased rate of prosthesis removal due to SSI post-chest wall reconstruction.10
Attention must also be given to pain control while changing the VAC dressing,11 which can be removed after resolving any systemic and local infection, and following at least two negative cultures.5 Usually, fewer complications, such as local bleeding and mild pain, are also noted during application of this modality. The use of VAC augments the standard treatment of infected wounds which is debridement and antibiotics, and better outcomes can be achieved if these are carried out in combination with each other.
Many thoracic surgeons think that the continuous suction of the VAC machine will interfere with respiratory mechanics and alter the intrapleural pressure.12 Theoretically, the intrapleural cavity is maintained in a net negative pressure throughout the respiratory cycle. Along with the atmospheric pressure, they oppose the elastic recoil of the lung, leading to its expansion. Moreover, the consistency and production rate of the pleural fluid also have an impact on the intrapleural pressure. Therefore, when the patient develops an empyema, in which a significantly higher production rate and higher viscosity of fluid take place, the intrapleural pressure is alleviated, thus affecting the respiratory mechanics.13 In respect of these two issues, negative suction will augment the respiratory mechanics. First, it regains the basal negative pressure by sucking the altered pleural fluid and clearing the space. Second, the net negative pressure it creates enhances lung expansion.
Another issue raised in this study was the communication between the pleural space and the intraperitoneal space, in the case of hiatal hernia, and which was managed surgically with a thoracoabdominal incision. The wound infection that was caused by oesophageal leak was managed by VAC dressing. Surprisingly, there was no interference at all with the respiratory cycle and the patient improved and was discharged from hospital.
From the literature, most of the papers appear to favour its safety and efficacy. It even reduces the need for the debilitating thoracoplasty procedure in such a case, thus preventing its associated perioperative morbidity and mortality.3
However, this study is unique in that the VAC was applied more deeply than is usually practised, in all patients, with the exception of two patients with empyema. In those two patients, the sponge was still inserted partially intrapleural. Sziklavari et al. described a similar technique in 2016.9 Our results showed that using a deeper suction within the pleural space did not negatively affect the patients' respiration, but rather enhanced a speedier recovery.
Limitations
This study has many limitations. It is an observational retrospective chart review. Lack of a comparative group may affect the recommendation. Further clinical randomised trials are needed to solidify the efficacy of this new technique.
Conclusion
The VAC technique is a revolution in the management of infected wounds and has proved itself in the field. Its deep use in thoracic surgery in the patients in this study, with complex and deep chest wall wounds, was safe and effective. However, further clinical randomised trials are needed to build the evidence base to support use of this new technique.
Reflective questions
- What are the possible complications of vacuum-assisted closure (VAC) therapy application to the open chest or to the pleural space?
- What should clinicians monitor in patients when a VAC dressing is applied?
- What are other adjunctive treatments to VAC dressing?
- What determines when the VAC dressing application should be ended?

